Local therapist Jo Warboys has put together a blog to support us with a plan to help us on what we can do to feel calmer in this time of uncertainty. Jo is also offering free telephone support to NHS and key workers.
Hello! During this time of uncertainty, increased stress & anxiety, this guide and plan may help focus on what you can do to feel calmer.
How you react and feel depends on many factors, including:
» the nature and severity of the personal impact of COVID-19 » experience with previous distressing events; » the support you have had in your life from others; » your physical health; » personal and family history of mental health problems; » cultural background and traditions; » age (for example, children of different age groups react differently).
We all have the strength and ability to cope with the current situation.
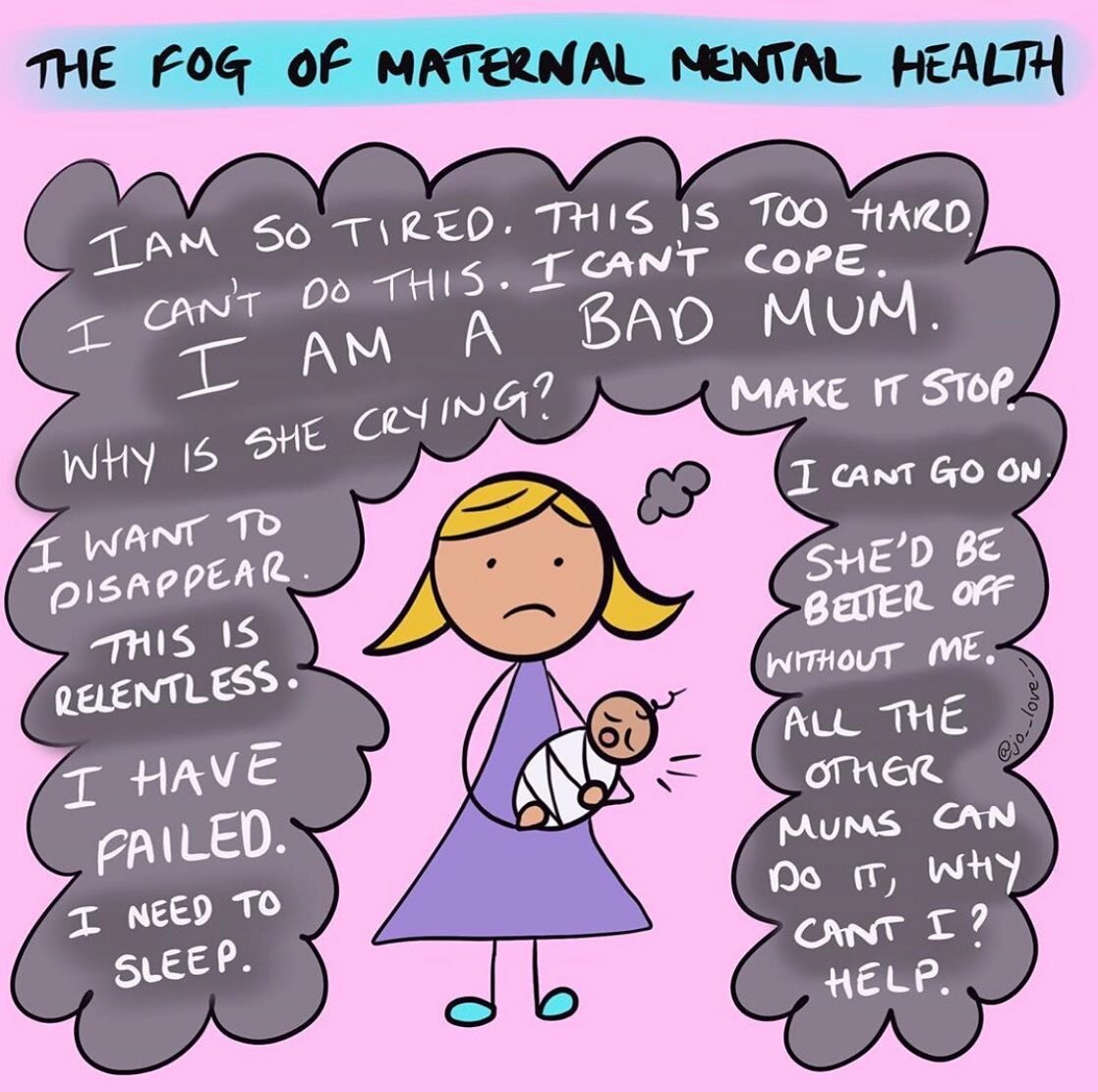
We may react in various ways to a crisis and/or an increase of stress. Some examples of distress responses to crisis are listed below: » physical symptoms (for example, shaking, headaches, feeling very tired, loss of appetite, aches and pains) » crying, sadness, depressed mood, grief » anxiety, fear » being “on guard” or “jumpy” » worry that something really bad is going to happen » insomnia, nightmares » irritability, anger » guilt, shame (for example, for not helping others) » confused, emotionally numb, or feeling unreal or in a daze » appearing withdrawn.
All these feelings are a reasonable reaction to what is going on right now. They are all coping mechanisms. You may feel them to varying degrees over a period of time.
Everything you feel is valid.
We have the ability to recover well over time with no long-lasting effects.
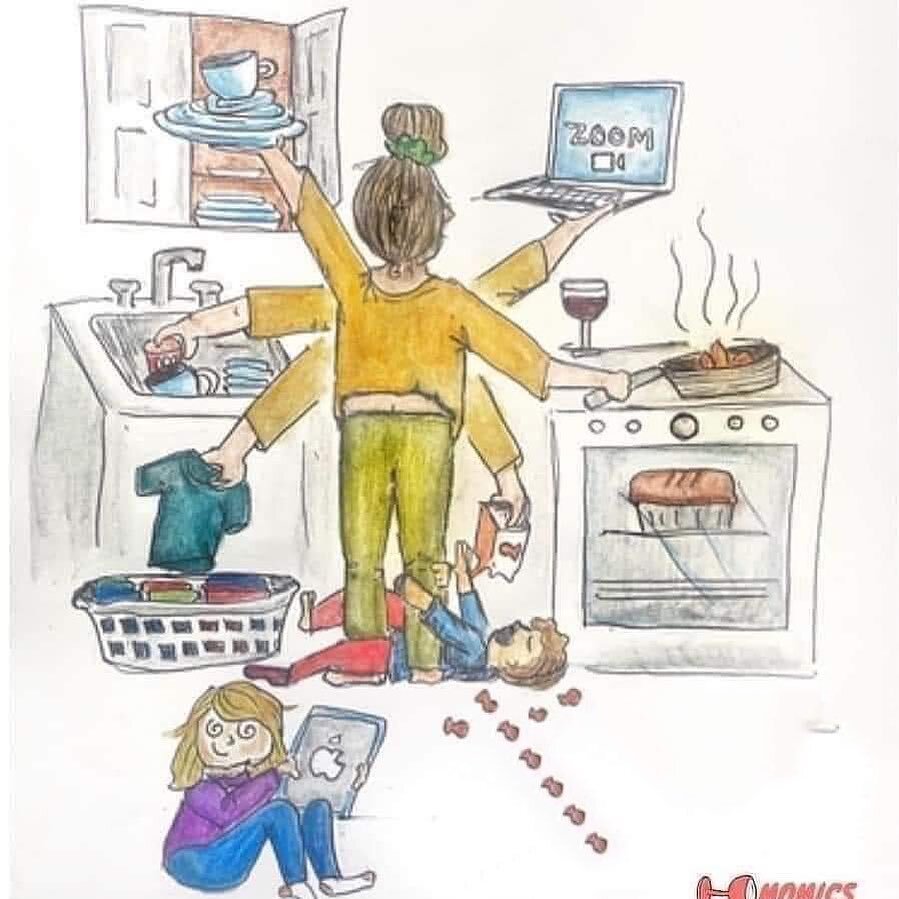
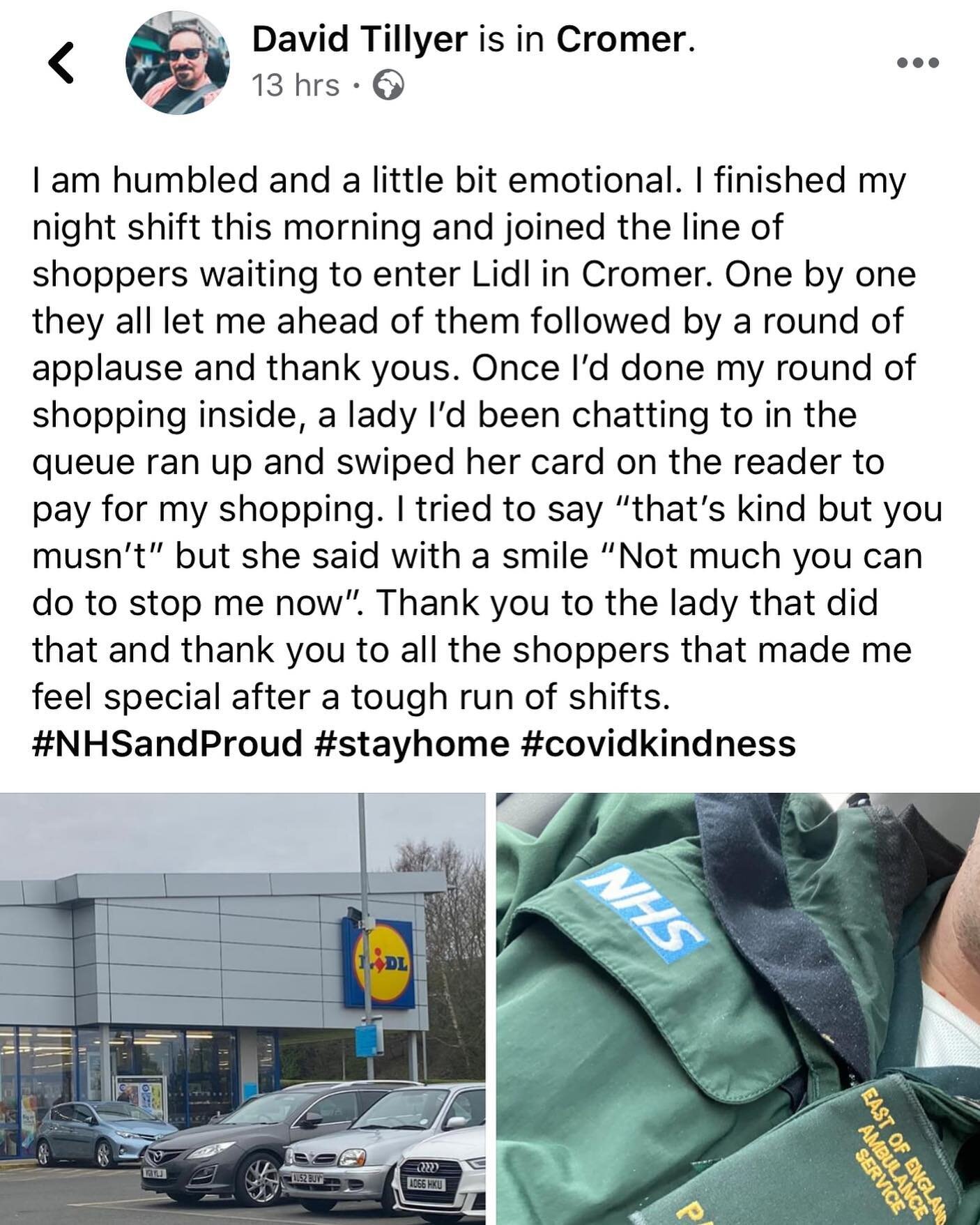
We all have natural ways of coping. I encourage people to use your own positive coping strategies, while avoiding negative strategies. This will help you feel stronger and regain a sense of control. I invite you to consider your positive coping strategies » Getting enough rest. » Eating as regularly as possible and drinking water. » Talk and spend time with family and friends via telephone, video call and letters. » Discuss how you are feeling with someone you trust. » Do activities that help you relax (walk, sing, play with children). » Do physical exercise. » Find safe ways to help others in the crisis and get involved in community activities.
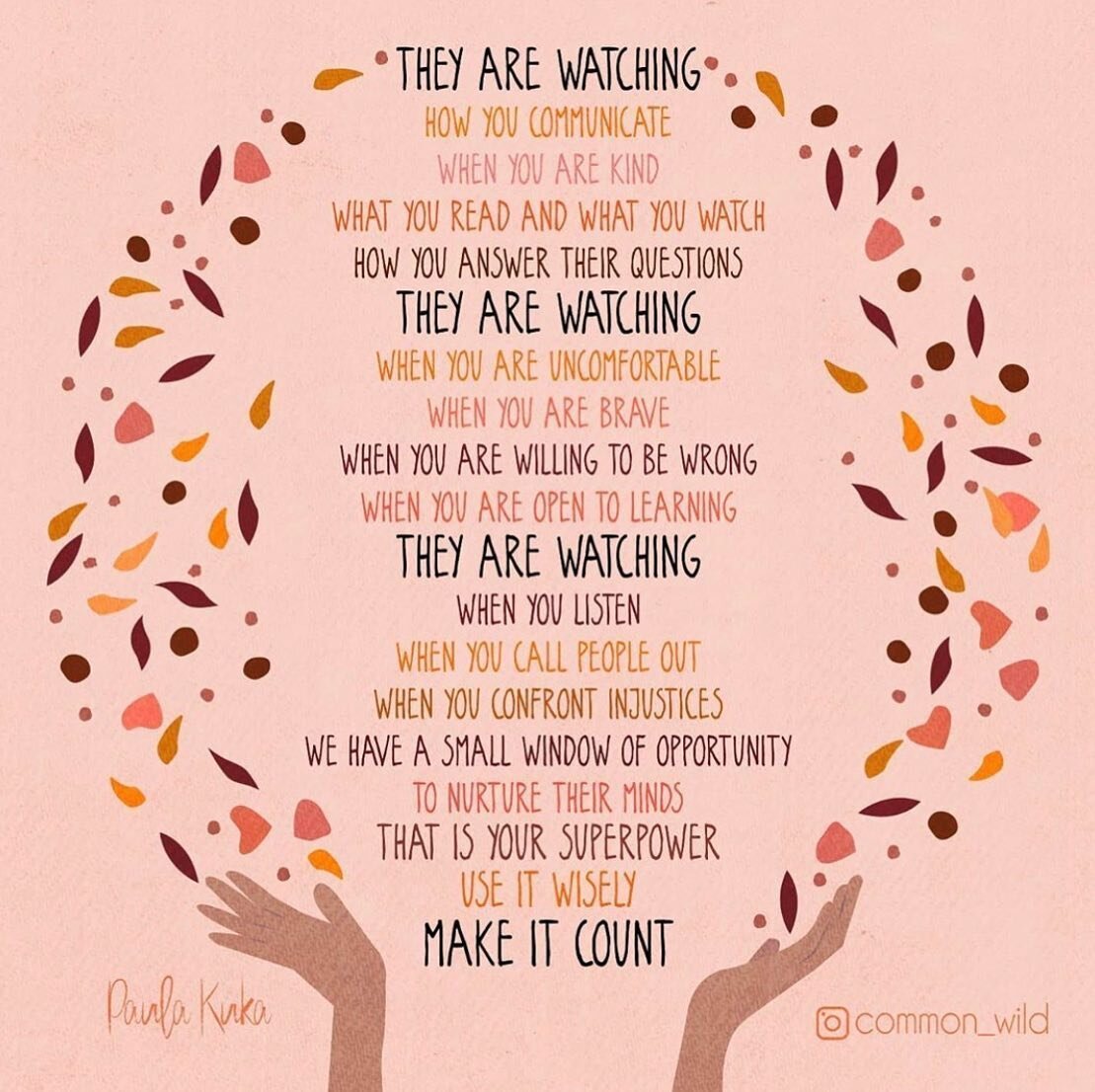
Things to say and do for children: stay together, Protect them from being exposed to any upsetting visuals » Protect them from hearing upsetting stories about what is happening. »Listen, talk and play » Be calm, talk softly and be kind. » Listen to children’s views on their situation. » Try to talk with them on their eye level, and use words and explanations they can understand. »
Remember that children also have their own resources for coping. Learn what these are and support positive coping strategies, while helping them to avoid negative coping strategies. Older children and adolescents can often help in crisis situations. Finding safe ways for them to contribute in the situation may help them to feel more in control.
During this, I invite you to use this plan to guide you through simple activities when you are feeling overwhelmed.
A self care / safety plan can help you avoid engaging in unhelpful, unsafe, out-of-control behaviour you may be accustomed to when under stress.
All our feelings are valid and we can work towards learning to sit with them all. We can choose activities that are safe, effective, and self-soothing. We can create the space to get to know what works for us and what does not.
This is YOUR plan, YOUR way of calming YOURSELF. There are no rules, no right or wrong, this is all about YOU!
Grab a notebook or piece of paper and work through the following steps:
STEP 1: What are your WARNING SIGNS?
What thoughts/feelings / behaviours let you know that you are struggling and need to use your self-care or safety plan?
Some examples include racing thoughts, tightness in your chest, feeling unloved, feeling panicked, tension with your partner.
Overeating, taking on too much, talking quickly, feelings of mania, digestion slows down, sleep is interrupted, feelings of panic and being trapped, can’t settle to 1 task at a time, difficulty prioritizing.
List yours in your plan
STEP 2: INTERNAL COPING STRATEGIES
What are some things you can do on your own to take good care of yourself?
This could include things like going for a walk, meditating, journaling, enjoying a cup of tea, eating a meal, lighting a candle, having a warm bath, reading, kitchen dancing!
Online gong bath, decluttering your wardrobe, sorting through papers and books, blow-drying your hair, get crafty, draw, paint…..
List yours in your plan.
STEP 3: SOCIAL SITUATIONS AND PEOPLE THAT CAN HELP TO DISTRACT ME.
When we are struggling we sometimes need to take a break and distract ourselves and/or regroup.
What are some things you can do that are with or around other people, if this is safe to do so?
How do we remain connected if we are self-isolating or socially distancing ourselves?
Connect online with a group, take an online fitness class, access an online yoga class, use social media to connect with others. Whatsapp group….
Write down other ways that you may find useful.
STEP 4: PEOPLE WHO I CAN ASK FOR HELP
At this point in the self-care and safety plan it is important to reach out and share with someone what you are going through.
Take some time now to think about who you will reach out to.
Do you have trusted friends or family members you could talk to? List yours in your plan.
STEP 5: PROFESSIONALS OR AGENCIES I CAN CONTACT DURING A DIFFICULT TIME?
Do you have any professionals in your life that you can reach out to?
Perhaps a talking therapist, teacher, or faith leader?
Peer Support network? Mental health websites?
If you are in crisis, here are some signposts to agencies and support.
Always know that they are available:
Government Coronavirus Information
Guide for adults on how to talk to children about the virus Mind Coronavirus information and well-being ()
Simplistic and friendly PDF guide to Coronavirus for kids
PLEASE DO TRY AND ENSURE THE INFORMATION YOU ARE EXPOSED TO IS BASED ON FACT AND VERIFIED.
This is a fluid plan and can change according to your needs. Thank you for taking the time to look after yourself.
References: World Health Organisation PFA, SHOUT Hive. NHS. Bisson, JI & Lewis, C. (2009), Systematic Review of Psychological First Aid. Commissioned by the World Health Organization (available upon request). Brymer, M, Jacobs, A, Layne, C, Pynoos, R, Ruzek, J, Steinberg, A, et al. (2006). Psychological First Aid: Field operations guide (2nd ed.). Los Angeles: National Child Traumatic Stress Network and National Center for PTSD. Freeman, C, Flitcroft, A, & Weeple, P. (2003) Psychological First Aid: A Replacement for Psychological Debriefing. Short-Term post Trauma Responses for Individuals and Groups. The Cullen-Rivers Centre for Traumatic Stress, Royal Edinburgh Hospital. Hobfoll, S, Watson, P, Bell, C, Bryant, R, Brymer, M, Friedman, M, et al. (2007) Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry 70 (4): 283-315. Inter-Agency Standing Committee (IASC) (2007). IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings. Geneva: IASC. http://www.who.int/mental_health_psychosocial_june_2007.pdf International Federation of the Red Cross (2009) Module 5: Psychological First Aid and Supportive Communication. In: Community-Based Psychosocial Support, A Training Kit (Participant’s Book and Trainers Book). Denmark: International Federation Reference Centre for Psychosocial Support. Available at: http://www.ifrc.org/psychosocial Pynoos, R, Steinberg, A, Layne, C, Briggs, E, Ostrowski, S and Fairbank, J. (2009).